Polycystic ovarian syndrome (PCOS) is characterized by chronic oligo- and/or anovulation, clinical and/or biochemical signs of hyperandrogenism, and/or polycystic ovaries detected by ultrasound. Three main phenotypes of PCOS have been proposed:
- Classic PCOS with hyperandrogenism and an-ovulation, with or without polycystic ovaries;
- Ovulatory PCOS with hyperandrogenism and polycystic ovaries; and
- Anovulatory PCOS without hyperandrogenism and with polycystic ovaries.
In PCOS, defects in insulin activity and secretion increase the risk of impaired glucose tolerance (IGT).
Insulin resistance in PCOS
It is now clear that PCOS is often associated with profound insulin resistance as well as with defects in insulin secretion. These abnormalities, together with obesity, explain the substantially increased prevalence of glucose intolerance in PCOS. However, these defects are also present in lean women with PCOS.
The insulin resistance in at least 50% of PCOS women appears to be related to the insulin receptor (serine phosphorylation/post-binding defect in receptor signalling). In fact, serine phosphorylation appears to modulate even the androgen biosynthesis. It is likely then this defect is responsible for both the insulin resistance and excess androgens.
In PCOS, fasting hyperinsulinemia is the result of a combination of increased basal insulin secretion and decreased hepatic insulin clearance.
Insulin resistance in PCOS has been associated with adiponectin, a hormone secreted by adipocytes that regulates lipid metabolism and glucose levels. Lean and obese women with PCOS have lower adiponectin levels than do women without PCOS.
Women with PCOS most commonly have postprandial dysglycemia, which reflects peripheral, primarily skeletal muscle, insulin resistance rather than fasting dysglycemia, which reflects increased endogenous glucose production. Therefore, 2-h post challenge glucose values are optimal for the diagnosis of IGT and Type 2 Diabetes in PCOS.
Similar insulin signalling defects have been identified in muscle and adipose tissue in PCOS and type 2 diabetes.
The defect in insulin action appears to be selective, affecting glucose metabolism but not cell growth.
Reproductive actions of insulin
1. Ovary:
Insulin is a reproductive as well as a metabolic hormone. Insulin receptors are present in normal and polycystic human ovaries.
It functions as a co-gonadotropin to modulate ovarian steroidogenesis. This action is preserved despite resistance to the metabolic actions of insulin in the periphery as well as in the ovary.
In PCOS there is selective insulin resistance in the ovary: decreased glucose metabolism and increased steroid hormone synthesis.
Increased insulin levels in synergy with luteinising hormone (LH) may arrest follicular growth that may contribute to anovulation.
It remains possible that there is increased sensitivity to the reproductive actions of insulin in PCOS because hyperandrogenism and anovulation improve during metformin treatment in women with PCOS without evidence for insulin resistance. Alternatively, these improvements may be related to a direct action of metformin on steroidogenesis.
2. Central nervous system (CNS):
Insulin signaling in the CNS also appears to be critical for ovulation. Genetic disruption of insulin signalling in the brain affects ovulation and body weight regulation.
Insulin resistance may result in decreased satiety in PCOS. Disruption of the neuronal insulin receptor results in diet-sensitive obesity, disrupted LH release, and impaired ovarian follicle maturation, suggesting that CNS insulin signaling is important for normal reproduction.
Insulin and Androgens
Polycystic ovaries secrete more androgens, in response insulin.
Insulin decreases hepatic production of sex hormone binding globulin (SHBG) causing elevations in free testosterone. In return, androgens can produce insulin resistance in women. This is seen when decreasing circulating androgen levels or blocking androgen action improves insulin sensitivity in women with PCOS.
Women who have Type 1 diabetes with PCOS are known to have some degree of peripheral insulin resistance due to exogenous insulin.
Insulin absorbed from subcutaneous depots results in relative peripheral hyperinsulinaemia and hepatic hypoinsulinaemia compared with normal physiology. Chronic adaptation to this combination could reduce peripheral insulin-mediated glucose uptake and increase hepatic glucose production.
Thyroid hormone and the ovary
Hypothyroidism (HT) may be associated with ovarian cyst formation. Hypothyroidism may also cause heavy, irregular menses, breakthrough bleeding, low endometrial thickness, ovulatory dysfunction, and sometimes non-proliferative endometrium due to anovulation.
Thyroid in PCOS: Is the prevalence of PCOS in women with HT higher than that in women without HT?
Thyroid disorders, especially Hashimoto’s thyroiditis and PCOS are closely associated.
Studies show that in PCOS patients, the mean level of TPO antibodies and the prevalence of clinically proven goiter were higher than those in controls without PCOS.
Thyroid and insulin resistance:
Hypothyroidism also has a component of insulin resistance.
Thyroid hormones are needed for glucose utilisation in the peripheral tissues. Lower thyroid hormones in plasma lowers the sensitivity of tissues to insulin. There is impaired translocation of GLUT-4 transporters on cell surface of adipose tissue and muscle.
Euthyroid patients on levothyroxine therapy and high levels of anti TPO antibodies show higher insulin resistance. This has been associated with a pro inflammatory state seen with autoimmunity.
Co occurrence of PCOS with Hypothyroidism: Mechanisms
1. Prenatal exposure:
Various factors such as high levels of estrogen or severe stress with increased cortisol in pregnant women could be responsible for the for the changes in the immune tolerance in the foetus and for the joint appearance of HT and PCOS in the adult life.
2. Genetic component:
It contributes an important part to the simultaneous development of HT and PCOS. Polymorphisms of the PCOS-related gene for fibrillin 3 (FBN3) could be involved in the pathogenesis of HT and PCOS. FBN3 is highly expressed in fetal tissues including fetal ovaries. Fibrillins influence the activity of transforming growth factor beta (TGFb).
TGFb is also a key regulator of immune tolerance by stimulating regulatory T cells (Tregs), which are known to inhibit excessive immune response. With lower TGFb and Treg levels, the autoimmune processes, well known in HT and assumed in PCOS, might jointly develop.
3. Vitamin D deficiency:
Vitamin D deficiency has been shown to be connected with the severity of thyroid autoimmunity and thyroid dysfunction. Vitamin D supplementation is supposed to improve menstrual frequency and metabolic disturbances in women with PCOS.
4. Estrogen-to-progesterone ratio:
Women with PCOS usually have similar estrogen, higher testosterone, and lower progesterone levels than women without PCOS. Consequently, their susceptibility to autoimmune disorders will probably increase because of a stimulating action of estrogens on the immune system. Therefore, the imbalance among estrogen, progesterone, and androgens may promote the occurrence of HT in PCOS women.
Take home
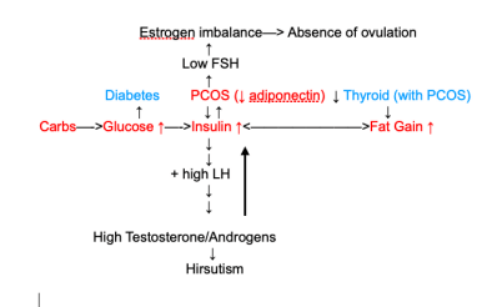
In short insulin resistance can cause and maintain PCOS. Harmful metabolic and reproductive effects are shown to be more pronounced in women with HT and PCOS.
Lifestyle changes directed at decreasing insulin resistance and total body fat will reduce adverse metabolic outcomes of hypothyroidism and hyperinsulinemia in PCOS.
References:
1. Thyroid and polycystic ovary syndrome
Simona Gabersˇcˇek, Katja Zaletel, Verena Schwetz, Thomas Pieber and Elisabeth Lerchbaum
European Journal of Endocrinology (2015) 172, R9–R21
2. Insulin Resistance and the Polycystic Ovary Syndrome Revisited: An Update on Mechanisms and Implications
Evanthia Diamanti-Kandarakis and Andrea Dunaif
Endocr Rev. December 1, 2012; 33(6): 981–1030.
3. The Polycystic Ovary Syndrome: An update on metabolic and hormonal mechanisms
R Dumitrescu, C Mehedintu, I Briceag, VL Purcarea, and D Hudita
J Med Life. 2015 Apr-Jun; 8(2): 142–145.
4. Study of Insulin Resistance in Subclinical Hypothyroidism
Sapna Vyakaranam, Swati Vanaparthy, Srinivas Nori, Satyanarayana Palarapu, Aparna Varma Bhongir
Int J Health Sci Res. 2014 Sep; 4(9): 147–153.
~Shweta Bhatia, Registered Dietitian, Mind Your Fitness