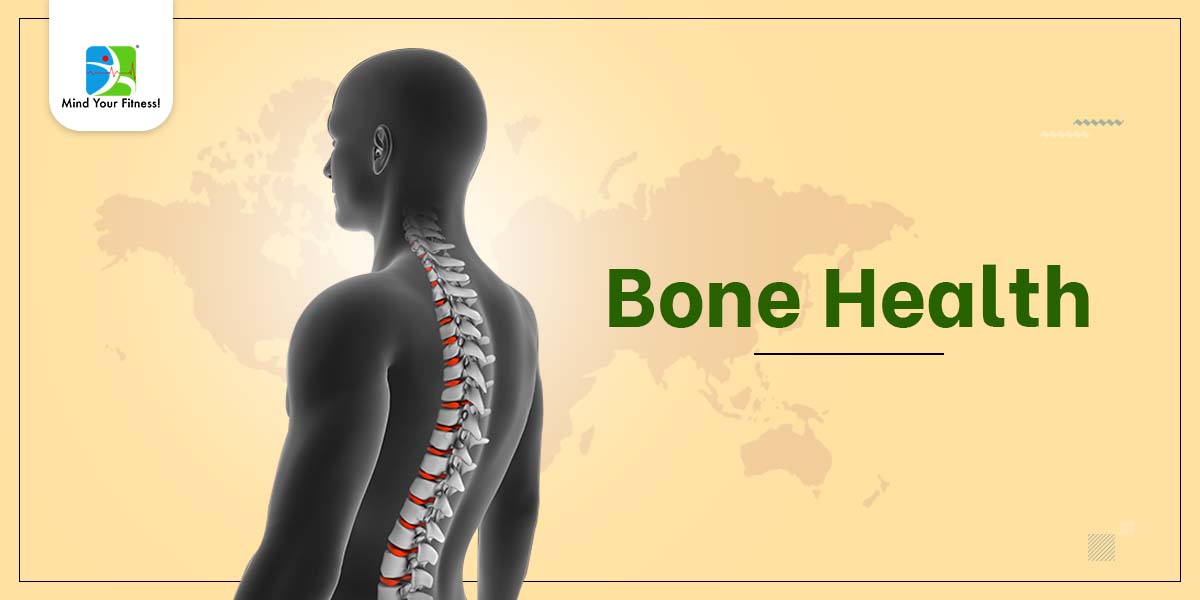
Osteoporosis, the skeletal disease of bone thinning and compromised bone strength continues to be a major public health issue. Bone fragility and increased risk of fractures especially hip and spine are characteristics of this disease. Risk for osteoporosis has been reported in people of all ethnic backgrounds. After the age of 70 years, both men and women have equal risk of suffering from osteoporosis.
Often osteoporosis is called ‘Silent Disease’ as bone loss happens without any symptoms. Fractures caused by either osteoporosis or low bone mass can lead to chronic pain, disability, as well as psychological symptoms, including depression. Bone health is optimized by creating an environment to achieve peak bone mass during adolescence, maintenance of healthy bone throughout life and prevention of bone loss with ageing. After the age of 30, losses exceed the ability to maintain bone mass.
The hormone oestrogen in women helps maintain muscle and bone. Menopause is accompanied by lower oestrogen levels leading to brittle bones.
Management
1. Diet:
Prevention of falls with maintenance of bone health through adequate calcium, vitamin D, and physical activity represent the base of the treatment for all individuals, including those with bone disease.
Calcium
Peak bone mass is usually achieved by age 30; therefore, physical activity and obtaining the recommended doses of calcium and vitamin D in adolescence and young adulthood will ensure peak bone mass development.
Dairy products (milk, cheese, cottage cheese and yogurt) are the best sources of calcium due to their high elemental calcium content, high absorptive rate, and relative low cost. Individuals who do not obtain enough calcium from foods should take a supplement to meet the age related guidelines.
In order to ensure adequate calcium intake, a number of calcium supplements are readily available. The two most common and well-studied calcium supplements are calcium carbonate and calcium citrate. To ensure optimal absorption, patients should be counselled based on the formulation and avoid interactions with food/other medications eg., thyroid hormone replacement.
Vitamin D
Main sources of vitamin D include sunlight exposure and supplements. As formation of vitamin D through sun exposure is based on several factors eg., cloud cover, use of sunscreens, skin colour, supplements are ideal to maintain levels. The desired adult level of vitamin D is 30 ng/ml (75 nmol/L) or higher.
Protein
Protein is an essential macronutrient for bone health. Protein makes up 50% of bone of which one third of bone and protein matrix undergoes continuous turnover and remodelling. First class proteins (animal sources eg., non vegetarian food and dairy) are essential to maintain this balance.
It is believed that a diet high in animal protein can lead to calcium resorption from bones. However, studies have found no increase in calcium losses on a diet providing 30% energy through protein. Increased protein intake may lead to increase urinary calcium levels due to increased absorption of calcium in the gut. One study found that among premenopausal women, there was a significant positive association between protein intake and bone mineral content, suggesting that dietary protein intake actually may be a determinant of bone mass. Clinical studies do not support the idea that animal protein has a detrimental effect on bone health or that vegetable-based proteins are better for bone health.
Concerns about the impact of animal protein on acid production appear to be minor compared with the alkalinizing effects of fruits and vegetables. Perhaps more concern should be focused on increasing vegetable intake and correcting calcium intake/Vitamin D status versus reducing good quality protein sources.
Protein and calcium intake are individualised and are dependent upon age, body composition, level and type of activity, fitness goals and existing health conditions.
Vitamin K
Studies have demonstrated that vitamin K2 can not only increase bone mineral density in osteoporotic people but also actually reduce fracture rates. Vitamins K and D work synergistically on maintaining bone density.
K2 is found in non vegetarian and fermented foods.
Other vitamins and minerals Vitamin A, B complex & C, and minerals like magnesium, phosphorus, manganese, copper, boron, iron, zinc and fluoride are also essential for bone health.
Crash diets and rapid weight loss without a structured exercise program are known to cause bone loss.
2. Exercise:
Role of weight bearing exercises : Numerous studies have shown that weight-bearing exercise can help to slow bone loss, and several show it can even build bone. Activities that put stress on bones stimulate extra deposits of calcium and nudge bone-forming cells into action. The tugging and pushing on bone that occur during strength and power training provide the stress. The result is stronger, denser bones.
Exercising if you have osteoporosis means finding the safest, most enjoyable activities for you given your overall health and amount of bone loss. There’s no one-size-fits-all prescription.
Consult your doctor before starting any exercise program for osteoporosis. You might need some tests first, including:
- Bone density measurement
- Fitness assessment
3. Medication:
Your doctor may prescribe certain medications based on the severity of bone loss and your age. Some of these may have interactions with food. Your healthcare expert/dietitian can guide you with that.
Take home message:
Starting early is the best but remember it’s never too late to start taking preventive measures.
~ Authored by Alifia Mala, Sports Nutritionist, Mind Your Fitness!